Clinical software integration faces challenges, but opportunities are on the horizon
Last updated on 28 November 2023

A research report from the Aged Care Industry Information Technology Council (ACIITC) has shed light on the full extent of the challenges and opportunities facing aged care providers when adopting clinical care software, with a lack of integration and consistent terminology and systems among the leading barriers to overcome.
Residential Aged Care Facilities Use of Clinical Care Software identified the need for more consistent data sets, coordinated strategies and greater accessibility for visiting healthcare professionals as some of the most pressing opportunities to take on.
Key points:
- In collaboration with the Australian Digital Health Agency, ACIITC collected data from representatives at 218 aged care organisations throughout 2021 and 2022
- The focus was on identifying the unique characteristics of all elements associated with the deployment and quality of the use of clinical care systems
- 287 unique clinical care systems were identified as being used by the sector, including instrumental systems focused on falls, serious incidents and care minute/financial reporting
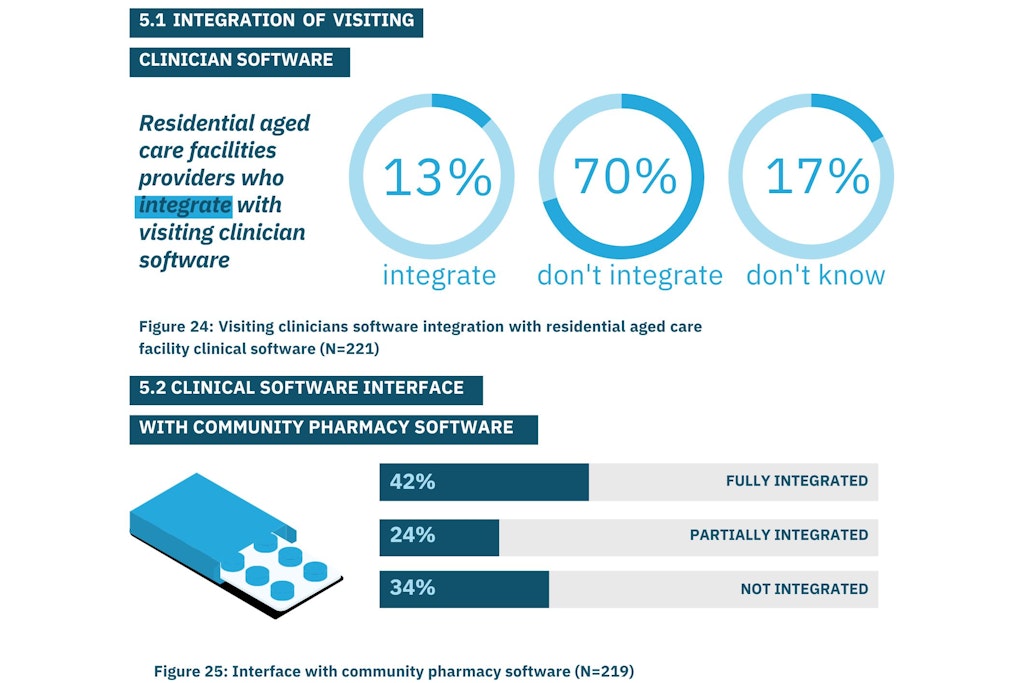
- 70% of providers said their clinical software cannot integrate with visiting clinicians’ software
- Less than 50% of respondents also indicated they provide training opportunities to their employees so they can access their clinical software with ease
Consistency is required
Without a coordinated approach to introducing new software or data collection, the aged care sector finds itself in a position where consistency is lacking. The Report identified 287 unique clinical care systems in use across 218 providers and ACIITC Executive Lead and Report co-author, Anne Livingstone, told hello leaders that much of the sector’s IT infrastructure requires an overhaul.
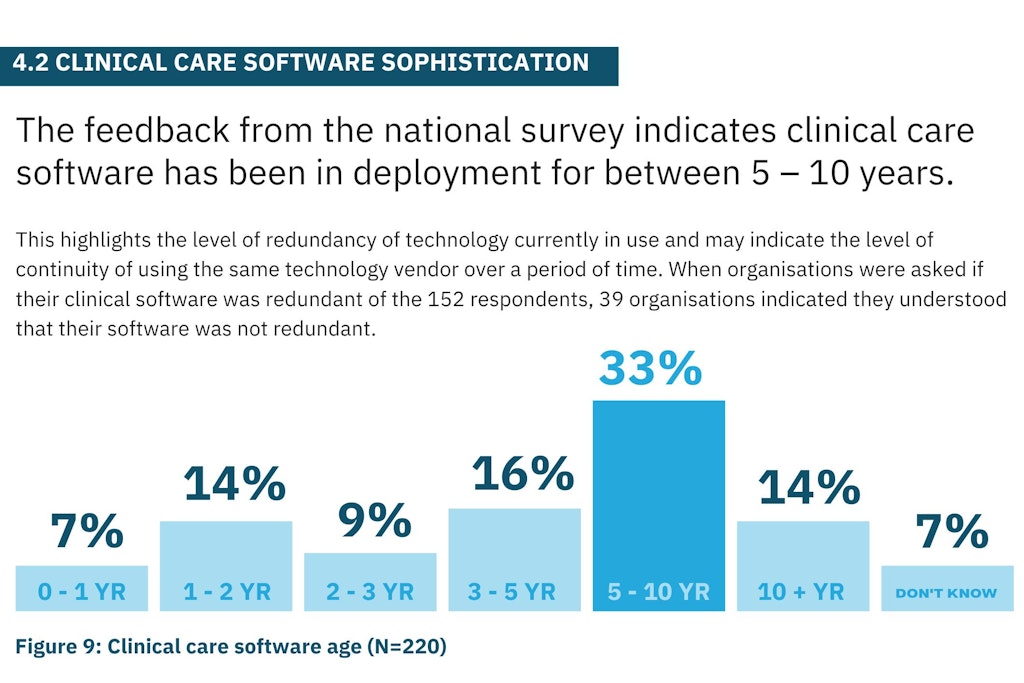
“We found some really innovative high-quality, high-class technology, but we did find a lot of technology has been in place for a long period of time – five years [or more],” Ms Livingstone said.
“If we overlay the advances in technology since COVID-19, for example, we’ve seen massive improvements in technology, particularly in remote monitoring technology. There is a need for many providers to review the systems and platforms they have in place and compare them to what the current market has on offer.”
“But of course that has a financial implication where many providers are financially stressed and the cost to invest in these technologies is relatively high. The workforce needs greater opportunity to improve its digital literacy and maturity and that in itself is quite a task but many providers are attempting to do that,” she added.
- One-third of the sector has been using the same clinical software for between five to ten years, while a further 14% said their software is over ten years old
- The cost of product, training and upgrading have been highlighted as some of the most common challenges to clinical software adoption
- Employee resistance and a lack of time and resources required for training and implementation were also cited as common barriers
Infrastructure diversity impacts integration
Limited integration and data standardisation among a diversity of technology infrastructure is arguably the preventing factor for aged care and healthcare interoperability with a variety of challenges and opportunities for improvement identified.
- Half of the respondent indicated their systems did integrate, 41% said they did not integrate, while the remaining 9% was unsure
- Almost two-thirds of respondents said there was no integration between medical, clinical and enterprise planning systems
- Only 42% of providers have clinical software that is fully integrated with community pharmacy software
- 77% of organisations have clinical software that does not record any data with resident information on My Health Record
“One of the biggest issues we found is the need for standardisation, and specifically data standardisation. This fits into some of the core Recommendations from the Royal Commission into Aged Care Quality and Safety, including Recommendation 68 which spoke to clinical systems being in place in residential care and having systems that met a certain standard set by the Australian Digital Health Agency. That standard is being developed,” Ms Livingstone explained.
ACIITC is currently researching and working on the development of technology and data standards for the aged care sector.
Meanwhile, although the lack of interoperability in aged care is a barrier to data management internally, it also impacts visiting clinicians, General Practitioners (GPs) and external agencies as they are prevented from seamlessly accessing and inputting data. Close to 39% of visiting clinicians do use clinical systems to review resident data but only 3% actually extract data.
Ms Livingstone also addressed the need to consistently collect quality data that will be used and analysed to its full potential.
“We see lots of scope to improve practice through the utilisation of data when it’s fully collected and standardised. The first stepping stone in improving any system is the need to standardise the collection of data, particularly the collection of data in relationship to the assessment of older people,” Ms Livingstone said.
Now is the time to plan for the future
There is plenty of opportunity on the horizon for aged care providers, and the Report recommended that providers invest in a technology and innovation strategy for the future. A clear strategy and development of clinical software guides will also support the implementation and training of staff, resulting in a more seamless process.
Ms Livingstone called for more Government guidance to support providers, and vendors, who require more insight into what the sector requires from technology and how it can implement it.
“There are some critical roles here for industry, but industry needs the roadmap from the Government. We still don’t know what the roadmap is for community care reform, for example, so how can people take the runway they need to get systems and processes in place if we don’t know what those reforms are going to look like,” she explained.
“But we see it as not just all challenges, there are possibilities and opportunities here. We’re very committed to seeing this project to fruition and seeing great strides within the standardisation of medical systems and the use of data.”