Is it reasonable? SaH providers face new battle with pricing expectations
Last updated on 1 April 2025

Home care service providers are about to become incredibly familiar with the term ‘reasonable’ after the Department of Health and Aged Care released a suite of Support at Home pricing resources.
Headlining the info dump is a summary of indicative Support at Home prices, an unassuming yet powerful document setting the tone for transparency over the coming months.
Older people accessing services, their families, carers and advocates now have a point of reference that could sway their attitude toward or away from a service provider if they think they’re paying too much.
Key points
- The indicative price ranges were collected through a survey in February. Over 300 HCP providers responded, representing over a third of all HCP providers.
- Indicative price ranges have been published to provide market-level information that will assist participants in understanding how a provider’s pricing compares with other providers across the country. They are not price caps nor recommendations.
- From 1 July 2025, Support at Home providers must publish their standard prices for all their services on My Aged Care. In addition, providers must keep evidence of what is included in their prices and be able to show the department or Commission when that information is requested.
From July 1, 2026, the Australian Government will step in and set price caps for Support at Home. Until then, home care providers shifting to Support at Home from July 1, 2025, have 12 months to continue setting their own prices.
These prices must reflect the costs of delivering the service and they must be reasonable. Yet in a sector where there are variations in contributing costs, what exactly is reasonable and justifiable?
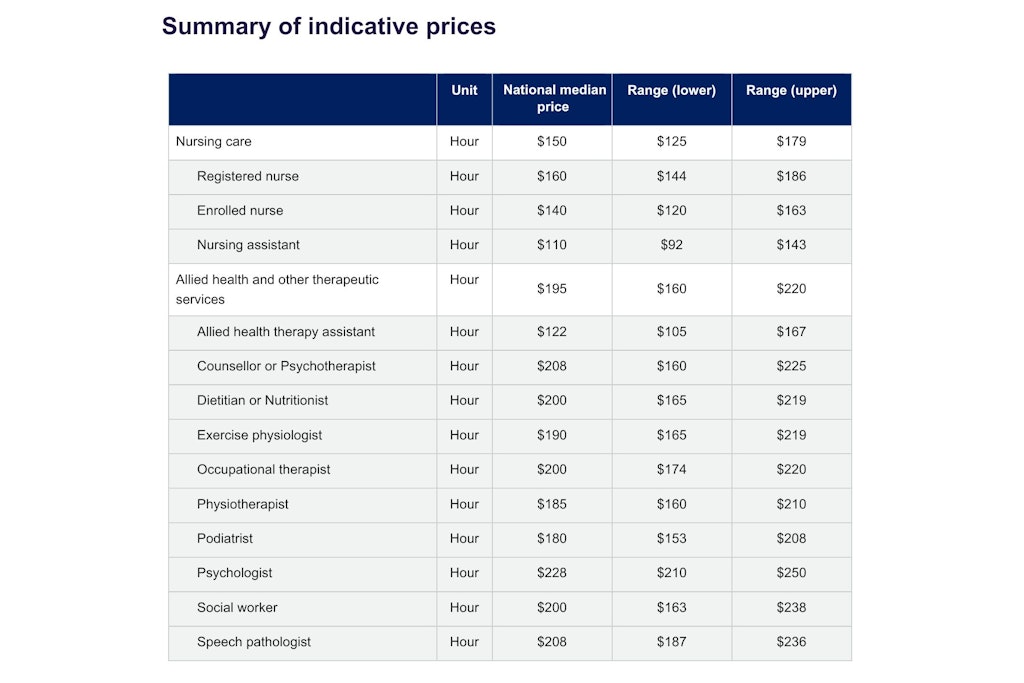
For nursing care (encompassing registered nurses, enrolled nurses and nursing assistants) the national median hourly price is $150. Lower range figures are around $125 and upper range around $179.
Meanwhile, the median price for allied health and other therapeutic services is $195, with a lower range around $160 and upper range around $220. Detailed breakdowns of individual services are included in the images below.
These are also the current prices set by HCP providers. They are likely going to be lower than what’s included under Support at Home because those costs will incorporate:
- Labour
- Package management
- Administration (e.g. human resources)
- Transport
- Sub-contracting, if applicable
- A margin to cover the cost of capital used in delivering the service
Prices can also reflect the costs of transitioning to Support at Home where they relate to the delivery of that service.
While the government will set price caps from July 1 next year, it will have to offer its own recommendations at some stage in the coming months. Providers require time to adjust and notify care recipients. There has been no confirmation yet when recommended prices are going to be released.
Additionally, there is no clarification of prices based on one of the most impactful determining factors: location. That means service providers could be faced with care recipients basing their expectations on the indicative pricing while ignoring the higher wages and contributing costs in thin markets.
Alex Lynch, Director of Public Health and In-Home Support, Catholic Health Australia (CHA), highlighted the issue when he said, “There is little delineation about the sample. It’s a third of providers, but no information about where they are, their size or demographics. Indeed, the prices are blended across rural and remote.”
“Some of the ranges are large, and the language suggests some prices were not included, without making it clear what the methodology for excluding them was.”
Mr Lynch said the department needs to ensure that messaging remains very clear to reinforce that indicative prices are a guide only and might not reflect final prices especially for those in higher cost areas.
Is this release a shock to the system?
Briefly looking at December 2024 average prices, Blue Bike Principal Consultant Luke Benson found that there has been a 30% uplift across the board with a 20% increase for nursing prices.
He said this is arguably lower than anticipated – and this could put providers in a good position moving forward with a realistic price cap from the government.
However, now that provider prices are out in the open, is it a shock for older people who have been unable to easily compare prices? Early reactions suggest a big yes.
G5 Principal Consultant Stephen Rooke summed up the issue best from a provider perspective when he said, “Isn’t it amazing that $30 per hour of carer wages turns into $100 per hour billable and $60 per hour for an RN turns into $160 per hour billable.”
“Who would have thought that years of doubling down on regulatory compliance and closing down avenues for investment in productivity gains would have led to such high admin and management costs. There were other ways to ensure more hours reach the end consumer, but here we are.”
If questions are raised about the gap between direct wages and the prices being charged, greater justification for what is deemed reasonable will be required. This is especially true for non-clinical care services that will include consumer co-contributions. Older adults want to know they’re getting value for money.
But the greatest challenge for pricing could occur when providers use contractors.
“One of the most challenging conversations in the sector is the ‘on paper’ gap between a care worker’s or care partner’s salary, and the “price list”. The fundamental problem is that pricing is a product of a ‘blended workforce’, and given 40%-50% of all service hours are delivered through brokerage, providers aren’t in control of the total cost. They have to pay the market rate for outsourced services half the time,” Mr Benson added.
“I know this isn’t an easy conversation, and the proper explanation feels very “commercial” instead of being person-centred, but we need to help ourselves as a sector by sharing a common understanding that there is NO evidence of price gouging going on at all – the margins are super lean and 100% of people in the sector are here to improve lives, not get rich and definitely not to exploit their staff.”
What are unreasonable prices?
The department also released a new fact sheet on consumer protections for Support at Home prices that accurately describes what it claims are ‘unreasonable prices’.
It states that prices must take into account all the funding a provider receives from the government to provide care. For example, if a provider receives subsidies or grants to deliver services in rural or remote regions, prices must reflect that funding.
An unreasonable price would also be if a provider charges separately for package management, travel expenses or asks for co-contributions to clinical care.
With all standard provider prices published via My Aged Care from July 1, 2025, the public will have more opportunities to compare prices and provide their own judgement on what is reasonable or unreasonable.
Meanwhile, if any changes to prices are to occur from this July, they must be clearly explained. All care recipients must agree to these prices as part of a new service agreement. Support at Home services cannot continue/begin if a service agreement is not signed.
Under Australian Consumer Law, providers cannot make misleading or deceptive statements about their prices, or the reasons for a price change. The Australian Competition and Consumer Commission can investigate and act where businesses mislead participants about prices.
If someone believes that the prices their current provider is charging is unreasonable, the department suggests the option of choosing another provider.
“It is important that you choose a provider who can deliver care that is right for you, that you have been approved for (as outlined in your Notice of Decision), and at a price that you think is reasonable,” it stated.
Where are the self management costs?
Aged care activist and advocate – and self-proclaimed agitator – Gwenda Darling also highlighted a notable missing feature: self management pricing guidelines.
As per the department, “The price for a Support at Home service is the entire cost of delivering that service.” This means it is the total amount charged to a recipient’s budget inclusive of package management, third-party costs and staff travel.
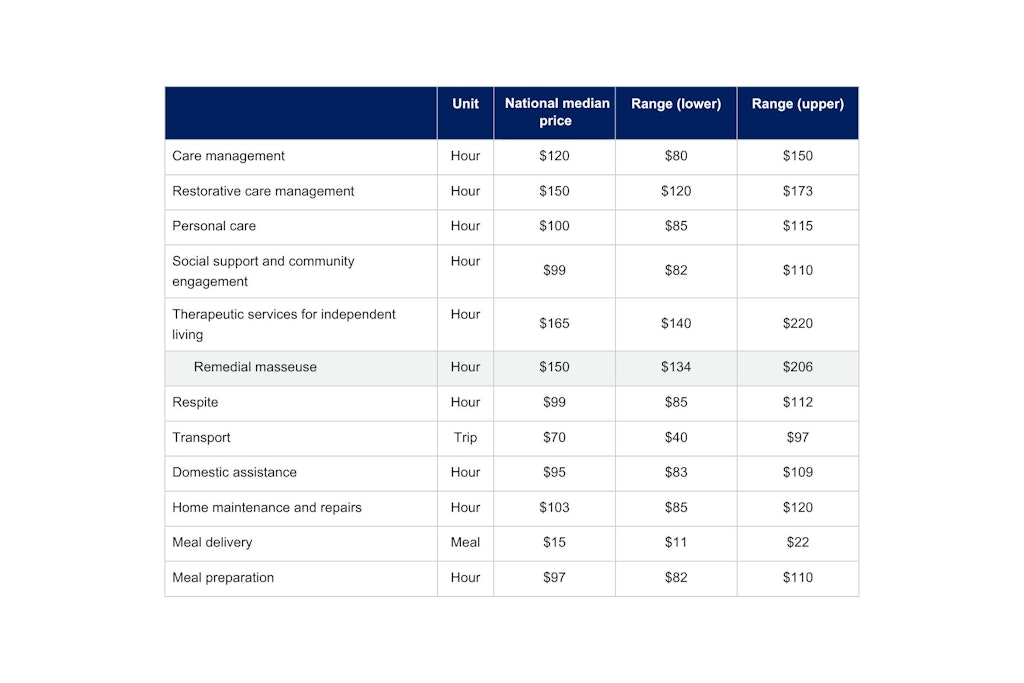
Yet it is not mentioned in the document that the indicative prices could be lower than expected as they do not include care management expenses. This could be setting some providers up to fail if older people are comparing prices to a median price without care management costs that range from $80-$150 per hour.
Denise Abraham, an aged care commentator on LinkedIn, called for the government to recognise self-management in the new Aged Care Act.
“Self management has grown exponentially in the last few years reflecting the change in the ageing process. People are living longer with failing bodies and still with full mental capacity. For reasons we can only speculate it remains mostly overlooked. There should have been a Section in the new Act dedicated to self management,” she stated.
“Instead, government preferred to continue the folly of eroding it and expecting it to be governed by the same legislation, and thinking, as full service management. Instead of acknowledging the new ageing process, government and businesses have decided to have a homogenised view of the aged and overlook self management. Shame. Government could have provided a win/win for business and the aged by moving with the changes in ageing.”
The information provided via the Support at Home pricing resources is not meant to challenge the sector. However, early responses from industry insiders suggest that setting reasonable prices will not be straightforward with so many competing factors and perceptions.