A roadmap to continuous improvement for Australian care providers
Last updated on 2 February 2024

Key principles of continuous improvement
The continuous improvement methodology is a systematic and ongoing approach to enhancing products, services, processes, or practices.
The fundamental principle behind continuous improvement is the organisational wide pursuit of incremental and sustainable enhancements rather than large disruptive overhauls. In addition to incremental enhancements, the continuous improvement methodology places importance on customer centricity, data driven decisions and cyclical iterative processes.
Organisations are encouraged to put the needs of customers at the centre, set goals, implement changes, measure outcomes and repeat the cycle over and over again. Each iteration builds upon the lessons learnt and improvements achieved from the previous one.
Continuous improvement methodologies and tools are widely used in various industries. Some of the most popular methodologies include Plan-Do-Check-Act (PDCA), Kaizen, Lean, Six Sigma, TQM, and Agile.
Implementing Continuous Improvement in care
Implementing Continuous Improvement in care requires a systematic and multi-faceted approach. Here are some practical steps and strategies that we recommend:
1. Establish clear vision and priorities
Establishing a strong culture of continuous improvement requires leadership commitment to define a clear and compelling vision that is backed up by specific goals and priorities.
Candidates for continuous improvement initiatives should be sourced from a broad range of areas including:
- Regulator audit outcomes and assessment
- Internal audits and inspection
- Incidents, hazards and near misses reported
- Client and staff feedback
- Business strategy and objectives
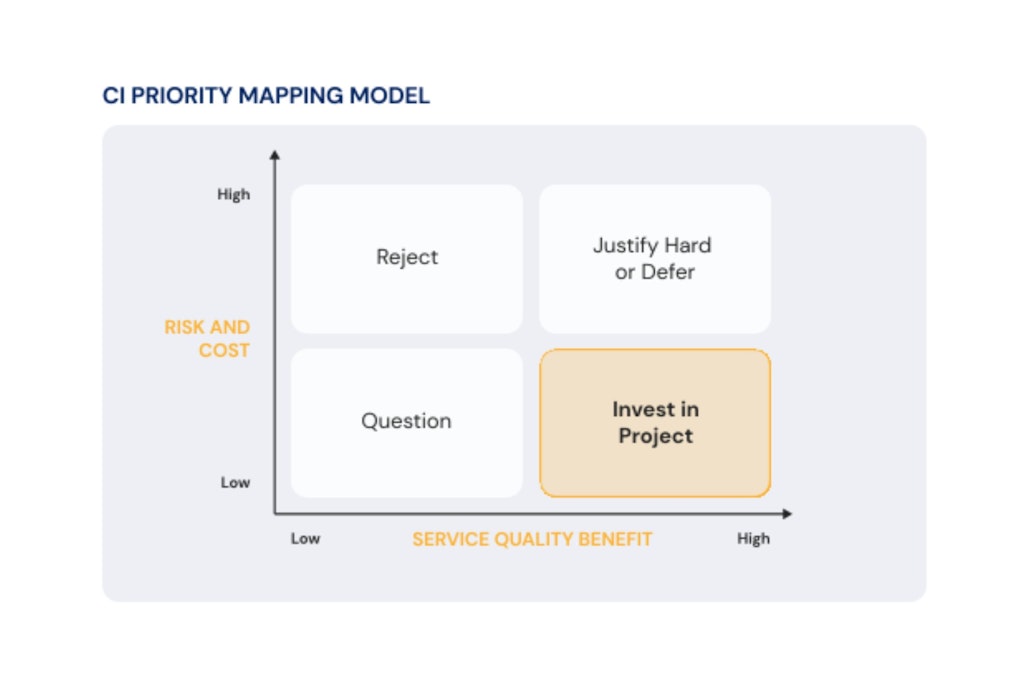
To prioritise, we recommend evaluating each initiative within a prioritisation matrix based on impact on customer and business outcomes. In doing so, it is critical to keep the most important principle of Continuous Improvement front of mind at all times: the focus on incremental and ongoing enhancements NOT large disruptive overhauls.
2. Adopt and train staff on a continuous improvement framework
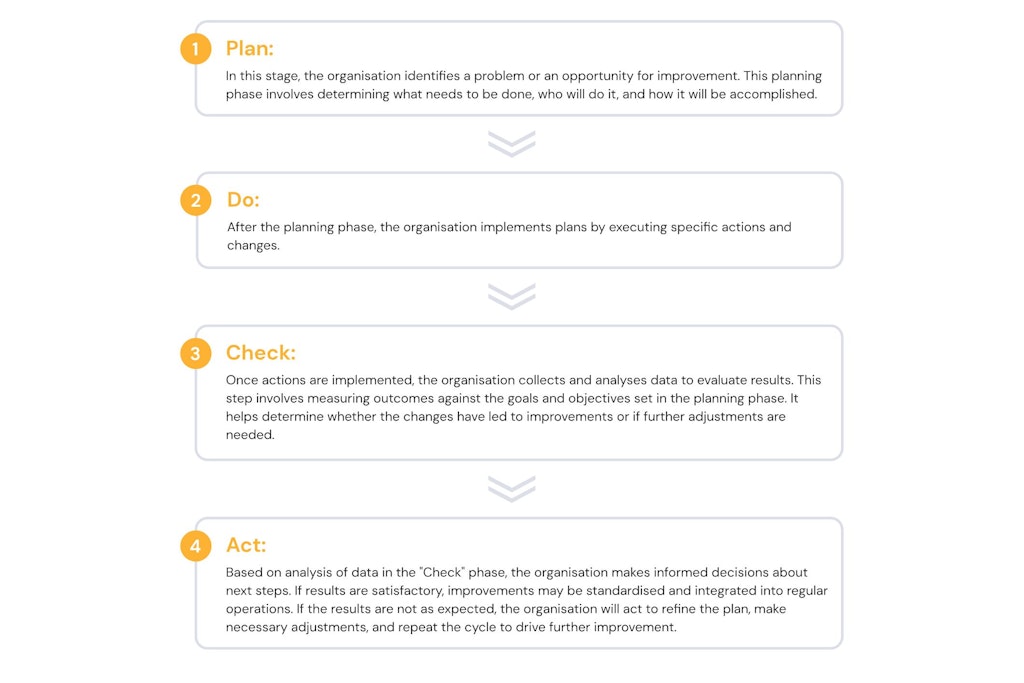
At Riskteq, we recommend the Plan-Do-Check-Act (PDCA) continuous improvement framework. It was developed by Dr W. Edwards Deming, a renowned statistician, professor, author, lecturer, and consultant who made significant contributions to the field of quality management. This framework is also recommended by the Aged Care Quality and Safety Commission.
The PDCA cycle consists of four main stages, which should be executed in a cyclical manner.
3. Plan: Define SMART goals and objectives
A clear and compelling vision with defined priorities should flow down into well documented, specific, measurable, achievable, relevant, and time-bound goals.
Here are some practical insights to get started with SMART goals:
- Be specific. Categorise improvements and objectives into key areas like resident care, safety and staff training. Clearly define each objective so that it is unambiguous and easy to understand. Specify the desired outcome and end state. Example: “Improve consumer satisfaction with meal choices in the dining area.”
- Ensure objectives can be quantified and measured. Example: “Increase the resident satisfaction score related to meal choices from the current 3.5 to 4.5 on a 5-point scale within six months.”
- Make sure objectives are attainable and supported with appropriate resources. Consider the available budget, staff, and time. Example: “Hire additional kitchen staff to support new menu options and dining area improvements.”
- Outline how each objective is relevant to the organisational vision and mission. Example: “Improving meal satisfaction aligns with our commitment to providing high-quality resident experiences.”
- Set a clear time frame or deadline for achieving each objective. This helps create a sense of urgency and provides a specific timeframe for assessment. Example: “Achieve the target satisfaction score of 9.5 within six months, with monthly progress reviews.”
- Document the objective and share it with relevant stakeholders within the organisation.
4. Do
Executing the ‘Do’ phase well requires thorough preparation, an empowered workforce and a critical focus on starting small. We recommend:
- Starting with pilot projects. This allows for testing the proposed changes in a controlled environment before rolling them out on a larger scale. Starting small helps to identify any unforeseen challenges, refines the implementation process and minimises potential disruptions to the organisation.
- Engaging and empowering employees to take ownership of their respective tasks, fostering a sense of responsibility and accountability. Encourage open communication, and actively seek input and feedback from those directly involved in the implementation.
- A strong focus on accurate documentation. Document the execution processes and any changes. This documentation serves as a reference for future endeavours and helps standardise procedures for consistency. It also facilitates the transition from the “Do” phase to the “Check” phase, where the outcomes are assessed.

5. Check: Leverage continuous and real time feedback loops
Feedback loops are crucial to inform all phases of continuous improvement. They are especially important at the Check phase because they provide a mechanism for gathering information, evaluating performance, and making informed adjustments. We recommend that care providers:
- Actively seek feedback and create multiple feedback mechanisms and channels that allow staff, residents, and their families to contribute insights. These may include in-person meetings, suggestion boxes, written surveys, digital forms, and dedicated feedback sessions.
- Offer anonymous feedback mechanisms for those who may be hesitant to share feedback openly. Anonymous channels can help people feel more comfortable expressing their concerns.
- Conduct regular surveys and questionnaires to gather structured feedback. These can cover a range of topics, such as quality of care, safety, staff performance, meal satisfaction, and overall resident experiences. Ensure survey questions are clear, concise, and relevant to the aspects being assessed.
- Establish resident and family councils where residents and their families can voice concerns and provide input. These meetings should be scheduled and facilitated by trained staff members who can actively listen and address issues.
- Place feedback forms and comment boxes in common areas, such as reception or dining rooms.
- Ensure digital platforms for feedback collection are user friendly and accessible to all, including those with limited technology skills.
- Implement real-time feedback mechanisms such as live chat that allow residents and families to provide immediate input or express concerns as they arise. Assign staff to respond promptly to real-time feedback, addressing issues or concerns in a timely manner.
- Assess staff engagement and satisfaction during the implementation of changes. Engaged and satisfied employees are more likely to embrace new practices and contribute positively to the improvement process. Address any concerns or challenges to maintain a motivated workforce.
6. Check: Analyse data and monitor performance
With multiple feedback loops and sources of real time data, organisations must get incredibly efficient at turning data into useful and actionable information based on well established evaluation criteria and KPIs. We recommend that care providers:
- Integrate systems and centralise data to build a single view of quality and continuous improvement plans across all facilities. Ensure data is accurate, complete, and up-to-date through appropriate system integrations, staff training and data integrity controls.
- Define and monitor key performance indicators (KPIs) such as resident satisfaction, incident reports, health outcomes, and staff performance. Leverage comprehensive reports and dashboards to identify trends, areas for improvement, and set benchmarks for performance.
- Implement automated alerts and triggers that notify staff when specific thresholds or criteria are not met, indicating a need for attention. This allows for early detection of emerging trends or potential problems, enabling timely intervention.
- Provide training and resources to staff on how to interpret and use data for decision making. Ensure they understand the relevance of data to their roles and responsibilities. Offer decision support tools and guidance for staff at various levels within the organisation.
- Regularly self assess and compare performance against industry benchmarks and similar providers.
- Document lessons learnt and communicate results. Effective communication of the results is paramount to the success of the “Check” phase. Clearly articulating the findings, both positive and areas for improvement, ensures that the entire organisation is informed. Transparent communication builds trust and creates a foundation for collaborative decision-making moving forward.
7. Act
- Prioritise action items based on their impact on resident care, operational efficiency, and overall organisational goals.
- Engage all relevant stakeholders to define action plans including staff members, residents, their families, and external partners.
- Implement changes incrementally. As previously discussed, embrace the iterative nature of the PDCA cycle. The iterative approach allows for ongoing refinement and optimization based on continuous learning. Incremental changes are also less disruptive to daily operations.
- Provide ongoing training and support. If the improvements involve changes in processes or procedures, provide ongoing training and support to staff members. Ensuring that employees are well-trained and supported in adapting to new practices enhances the likelihood of successful implementation.
- Regular assessments and adjustments. Leverage established mechanisms for continuous monitoring of progress throughout the implementation of action plans. Regularly assess whether the changes are producing the desired results and whether any adjustments are needed. This ongoing monitoring allows for real-time adaptation.
- Acknowledge and celebrate achievements and milestones reached during the implementation of action plans. Recognizing and rewarding progress boosts morale and motivation among staff members, creating a positive environment for ongoing improvement efforts.
8. Repeat
As the Act phase concludes, transition seamlessly into the planning phase for the next PDCA cycle. Based on the outcomes and lessons learned, set new objectives, refine strategies, and plan for further improvements. This cyclical approach ensures that the organisation is continually advancing in its pursuit of excellence.
Riskteq software for Continuous Improvement in care
Riskteq software enables customers to build an integrated continuous improvement system to enhance quality of care. It is built from the ground up to implement PDCA continuous improvement workflows with an established track record in the Australian Care industry.


Riskteq’s approach to managing change
Although new processes or technology may be involved, the efficacy of any continuous improvement initiative hinges entirely on individuals and their capacity to comprehend and endorse the associated changes.
Passive resistance has the potential to undermine even the most well-intentioned programs. Consequently, engaging individuals in the transformative process is paramount for success.
Riskteq’s human-centric approach to continuous improvement emphasises clear communication, adept stakeholder management, and facilitating a comprehensive understanding of the vision’s value for both individuals and the organisation.

About Riskteq
Proudly made in Australia, we enable organisations to link business objectives like high quality of service with risk prevention, incident management, feedback and continuous improvement initiatives. For more information please get in touch with us at [email protected] or call +61 3 6230 4833.