Integrated care sectors a focus in new Mental Health Workforce Strategy
Published on 11 October 2023 (Last updated on 20 October 2023)

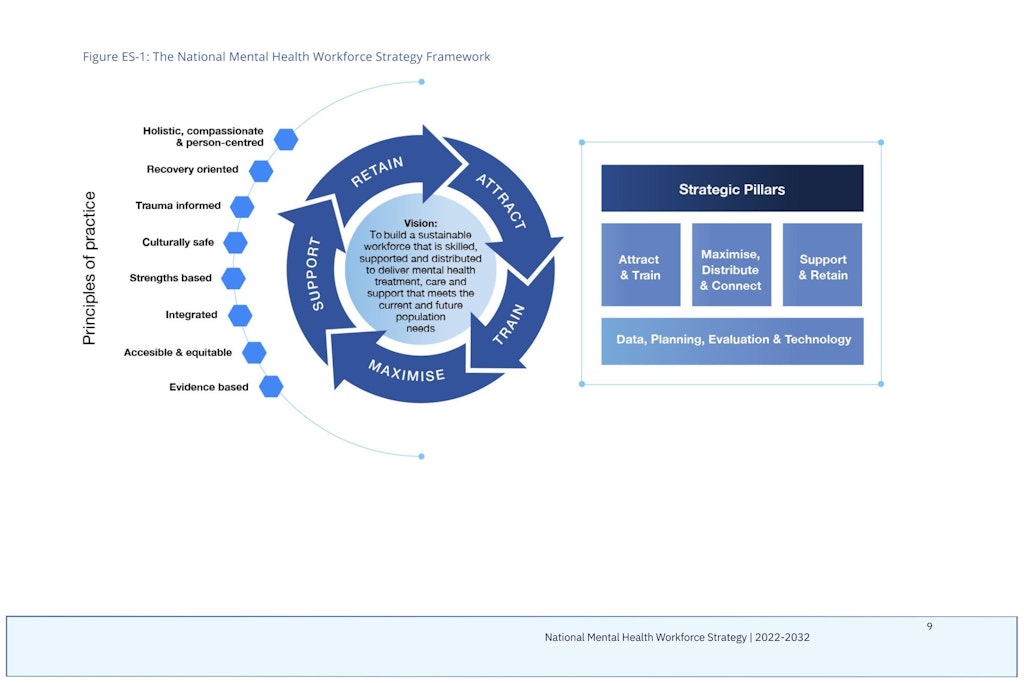
The Federal Government has released the National Mental Health Workforce Strategy 2022-2032 as a guide to build and strengthen Australia’s mental health workforce. Although the focus is on the mental health workforce itself, overlapping needs with the aged care workforce indicates the Strategy will have a notable impact on the care economy as a whole.
Key points
- The mental health workforce includes those working exclusively in the sector and those who frequently treat, interact with, care and support people experiencing suicidality, mental health distress and/or ill-health, including aged care workers
- Workforce shortages, unclear scopes of practice and limited examples of collaboration are key challenges listed by the Government
- $17.8 million will be invested to upskill the broader health workforce in mental health, which will include undergraduate nurses and allied health students
The Strategy has a broad focus on the challenges facing the mental health workforce as part of the care economy; one sector cannot see all of its problems solved in isolation. Many of the challenges identified are just like those in the aged care (and disability) sectors.
Both mental health and aged care require more investment in attracting, training, supporting and retaining staff. The workforce itself must be more sustainable and skilled than ever. Its full potential also has to be maximised for the current and future population; a future population that will require more support across the board.
“The quality of the mental health system relies on its workforce. Australians deserve a mental health care system where people can get compassionate help from highly skilled professionals,” Mark Butler, Minister for Health and Aged Care, explained.
“The Strategy is a first step in the Government’s long-term goal to ensure our mental health care system has the workforce in place to care for Australians needing mental health support.”
Attracting and integrating staff a priority
Much like aged care, the need to attract and train staff to boost the mental health workforce is seen as the greatest priority for the sector. In some ways, this may come at odds with aged care. Both sectors are looking for ways to entice nurses and healthcare workers by creating a more attractive and rewarding work environment.
However, the Government does not appear to be pitting the sectors against each other. It has acknowledged they overlap and an integrated workforce would provide long-term benefits such as minimising barriers to service and preventing individuals from falling through the gaps between sectors. The Strategy said ‘attitudinal, organisational and legislative barriers’ must be addressed to effectively achieve this.
Additionally, strengthening the rural and remote workforce to produce more homegrown professionals that can support smaller communities in various healthcare and aged care settings has been identified as a top priority. This focus has already been warmly received by the National Rural Health Alliance (the Alliance).
“We know mental illness in rural and remote Australia is more prevalent than in major cities and tragically, rates of self-harm and suicide increase with remoteness,” says Alliance Chief Executive, Susi Tegen.
“We are particularly pleased to see the reference to the need for homegrown professionals as the Strategy notes that people originating from rural and remote areas often have a preference to undertake training and employment in their own or comparable communities.”
“The Strategy rightly notes that there needs to be a focus on developing, growing and sustaining the regional, rural and remote mental health workforce through providing localised education, training and placement opportunities for students.”
Investments in strengthening the mental health workforce to better support culturally and linguistically diverse (CALD), LGBTIQA+SB (lesbian, gay, bisexual, transgender, intersex, queer, sistergirl and brotherboy) and First Nations communities would also provide a much-needed boost to the aged care industry. This is described as a ‘wrap-around’ model in the Strategy, which is essentially a person-centred care approach.
“We welcome the reference to wrap-around service delivery models that adopt a person-centred approach that includes their family and carers which have demonstrated the potential to improve health outcomes, particularly in regional, rural and remote areas. But we now need to see the resources and commitment by all levels of government to ensure the actions in the strategy become tangible responses to this area of critical need,” Ms Tegen added.
With a ten-year roadmap in place, the Strategy has established a six to ten-year timeline for integrating workforces and care pathways. Relevant aged care peak bodies and providers have been highlighted as key parties involved in the process with more details to come.