One-third of aged care employees want to leave, citing increased demands and regulatory burden
Published on 28 November 2023

Ideagen has released its annual Aged Care Workforce Report, claiming that the Government’s ambitious aged care reform agenda faces a reality check as staff struggle to meet increasing regulatory demands.
Additionally, in a sign of sector stabilisation, the workforce exodus appears to be slowing down although management loss remains relatively high. New hires are also placing extra pressure on experienced staff while direct care minute goals still seem to be out of reach for many providers.
Key points
- Four out of five workers have experienced an increased workload due to the introduction of the 2019 Aged Care Quality Standards. Extra training and supervision for new staff has compounded the problem
- Each resident receives an average of 180 direct care minutes per day, 20 minutes below the mandated 200 per day, with just 7% of staff saying the target is “easy to achieve”
- One-third of the workforce plans to leave the sector in the next three years, citing stress, excessive overtime/expectations and too much paperwork as top reasons for wanting to leave
- Remuneration, last year’s top concern, has dropped down the ranks following the 15% pay rise
Increased workloads and supervision
Additional regulation within the aged care sector has seen workloads increase for 82% of workers, which has been compounded by additional responsibilities with supervising and supporting new staff.
In total, 80% of workers said new staff require significant extra training/supervision, indicating many new staff are not necessarily ready for the job. Roughly one-third of this cohort is perceived as a risk to residents if they work without extra training or supervision.
“While almost all aged care homes have seen an influx of new staff this year, the new arrivals are too few and too inexperienced to meet the demands imposed by increasing and confusing regulation,” the Report stated.
Just 17% describe new staff as well prepared and further 3% very well prepared.

Care minutes are difficult to achieve
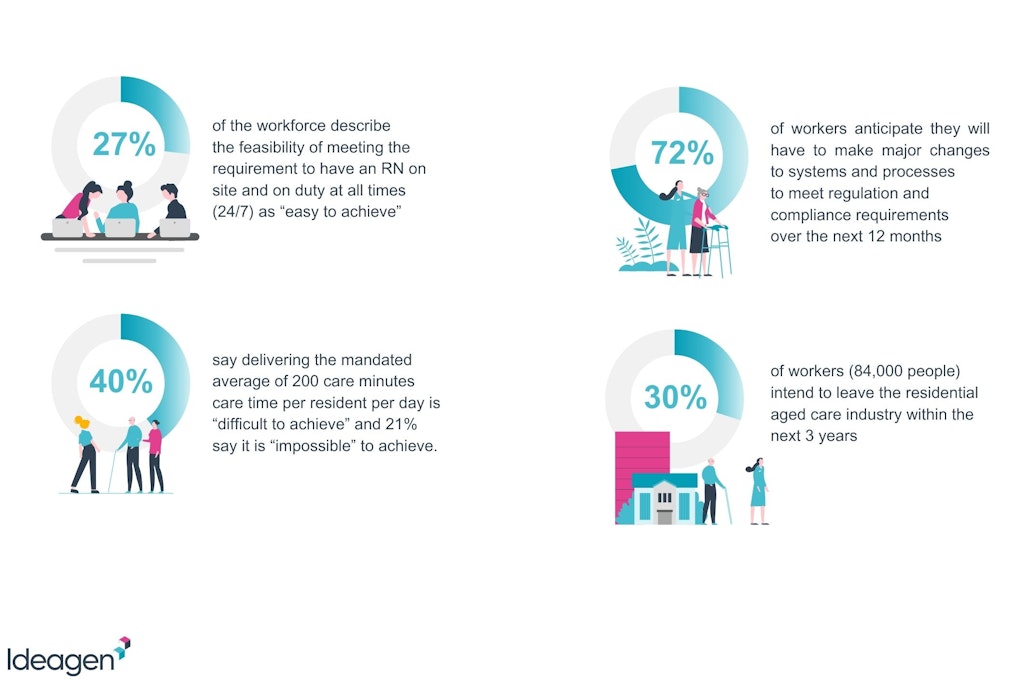
Recent data from Mirus Australia revealed the sector is averaging 209 direct care minutes per resident per day, however, Ideagen data indicates this figure is closer to 180 minutes. Staff hold pessimistic views of the mandates as two in five employees believe it’s difficult to achieve while one in five said it’s impossible.
“When considering the 200-minute care requirements, I have serious doubts about its feasibility. During my time working at a facility, we had only one Registered Nurse per shift responsible for almost 90 residents and occasionally two if there were numerous dressings to attend to,” said a Registered Nurse Care Manager.
“Unless the staffing issues are addressed, attracting competent and dedicated staff to this sector will remain a significant challenge.”
Just 27% of employees believe meeting 24/7 Registered Nurse coverage is easy, with a similar amount saying it’s impossible.
“These are only two examples of a broader trend where well-meaning reforms are imposing an ever-greater burden on the aged care workforce,” stated David Griffiths, Senior Vice President, Ideagen.
Reporting obligations are confusing
Mr Griffiths added that it’s not just the challenge of meeting obligations weighing heavily on providers and employees; a dizzying array of reporting has created considerable issues.
Just over half the workforce is confused by their reporting obligations, including what data has to be reported and when. The introduction of new technologies will hopefully make the administrative and regulatory process easier for staff, although 72% believe major changes to systems and processes are required over the next year.
This is partly due to the Aged Care Quality Standards being revised in 2024 and the introduction of a new Aged Care Act.
Management and staff loss continues
There has been a drop in staff wanting to depart the aged care sector. In 2022, Ideagen reported that half the workforce intended to leave within three years. Now, that has dropped to just one-third. While it’s still a concerning figure, it suggests that the post-pandemic era has brought stability back to the workforce.
The interim 15% aged care pay rise also played a significant role in staff retention. Almost one-quarter of staff said remuneration was their top reason for leaving in 2022 and 63% had it in their top three; this year those figures are 14% and 49%, respectively.
Unfortunately, management losses have not slowed down, with 41% of workers stating they have lost half or more of their management team over the past year. A small group, 8% of workers, have seen their entire management team depart.
“Growing gaps in leadership deprive workers of much-needed guidance and oversight from experienced managers which in turn undermines stability and workers’ capacity to provide continuity of care for residents,” the Report said.
You can access the full Ideagen 2023 Aged Care Workforce Report here.