Underreporting could prevent providers from achieving three-star Staffing Ratings
Last updated on 30 October 2023

Mirus Australia has dropped its October data release for the aged care industry with sector-wide care minute and Registered Nurse (RN) minute increases headlining a positive quarter of results.
The data, which reflects nearly one-third of the residential aged care sector, still shows a shortfall in RN care minutes despite the increase, and with Mirus finding that 92% of facilities are under-reporting their care minutes, millions in funded rosters are not being reported.
Key workforce data:
- Mirus reported that the sector-wide daily care minute average increased by 2.45% to 199.68, just shy of the required 200-care minute average.
- RN minutes experienced strong growth, increasing by almost 8% to 33.94 minutes per day. However, this is below the required 40-minute average.
- Based on the data, roughly 60% of the sector is under the required amount of direct care minutes or RN minutes to achieve a three-star Staffing Rating.
Come April 1, 2024, aged care providers will only achieve a three-star Staffing Rating if they meet their mandatory care minute targets for both RN minutes and total direct care minutes. Speaking to hello leaders, Mirus Australia Industry Lead Robert Covino said this should be a wake-up call for the majority of providers who are compliant today, but will not be next April.
“If we look at the achievement rates of the sector right now there’s about 60% of the industry under three stars. But if we look at it from a pure care minute mandate… and look at what percentage is actually compliant today from last quarter’s data set, it’s only 19%,” explains Mr Covino.
“That is a big gap from [the amount of facilities with] three stars. About 80.8% are under their total time or their RN time, or vice versa. Largely we’re seeing it’s usually the RN time that is not the one they are achieving across the sector.”
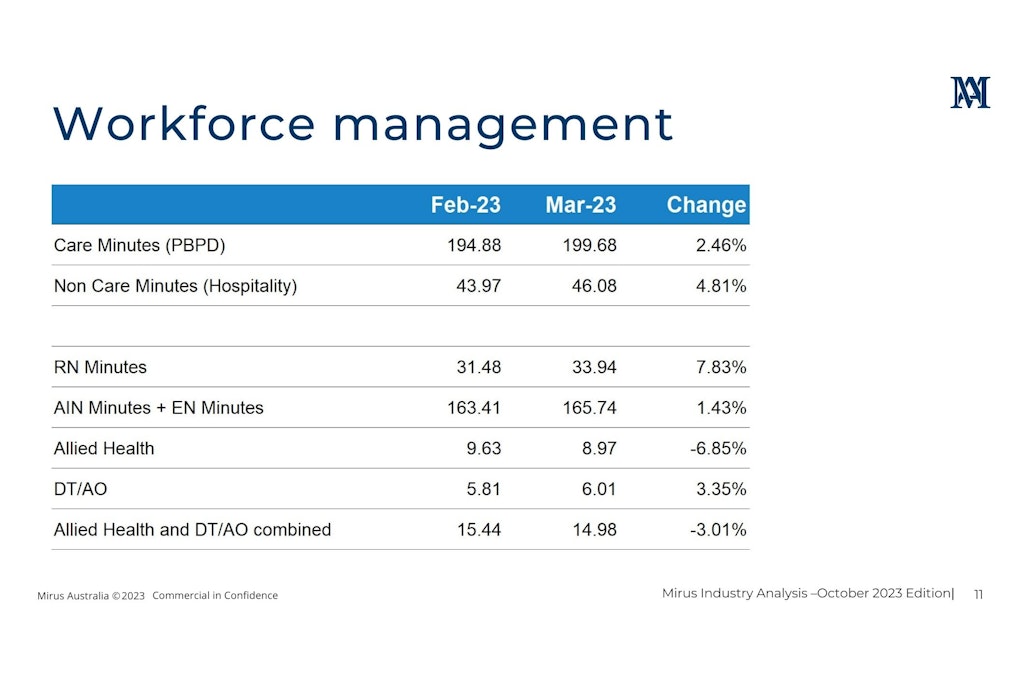
RN minutes have improved to 33.94 sector-wide, an increase of over two minutes since August. But in a sign that providers are closer than they think, nine out of ten are unknowingly under-reporting care minute data. In many cases, this is due to businesses not recognising key staff members providing direct care as it may only be a small percentage of their role.
For example, senior staff members who are qualified RNs could have a percentage of their activities included in RN care time reporting if it is a recognised task by the Government.
“We found that 92% of our actual clients are under-reporting. Given nearly 81% of the industry is not meeting their care minutes… perhaps the wages that they’re already expending and that time are already there and they just don’t know it yet,” explained Mr Covino.
“Close to 43% [of facilities] have a policy that references the allocated time as well as some of the activities they include for those positions and personnel, but none of the providers actually had the policies that related to the individual position description,” he added.
An updated position description linked to a care minute policy would highlight the work relevant to care minute reporting, alleviating some of the pressure in meeting care minute quotas.
Speeding up resident reclassifications
The Australian National Aged Care Classification (AN-ACC) funding model provides far more accurate funding allocations. Many providers have settled into the new revenue model with the understanding that claims maximisation is no longer the best way forward.
However, some providers continue to forge ahead with the old tactics of chasing the highest resident classification to receive increased funding. Mr Covino said this is not an effective method as driving up care minute requirements could harm facilities with fewer workforce resources.
Instead of viewing classifications as one-way, he said providers should acknowledge that effective models of care will lead to resident classification changes.
“We may have to move classifications backwards because providers can say ‘We did our job, we reabled somebody who was in a deteriorated state in their home and they were neglecting themselves and now they’re better’. That is a different approach to previous entitlement structures that were all about working to get that next level up for classification,” he explained.
“Maximising claims for the last 18 months through the shadow assessment period has created skewed casemix distributions where there’s arguably 10% more time required than would actually be represented in the site today. That’s fine if you have the resources.”
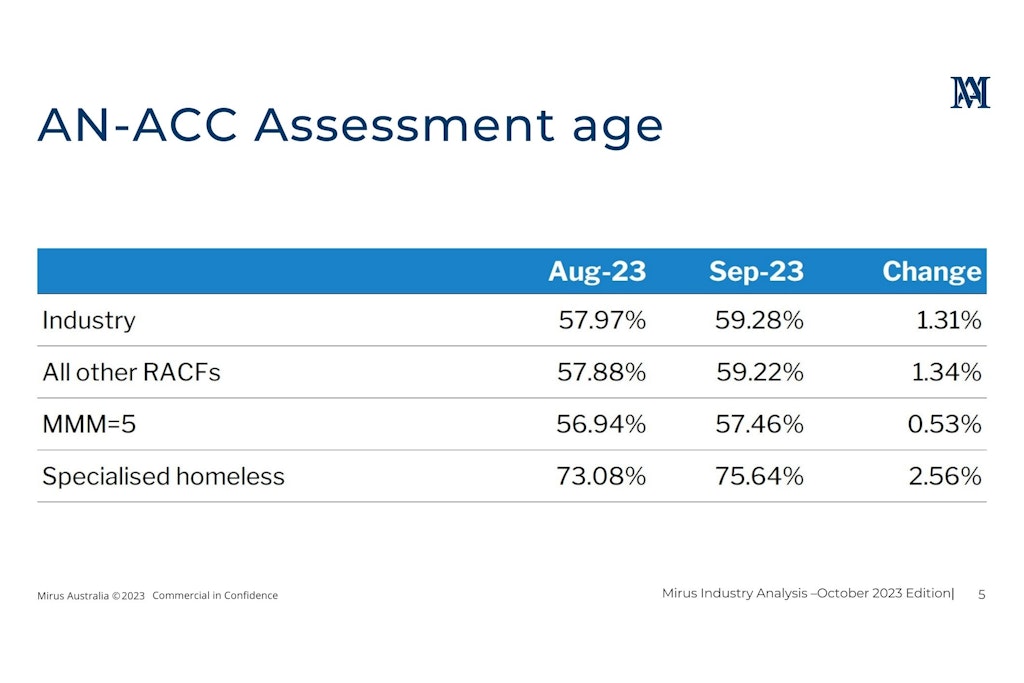
One of the key metrics recorded by Mirus is the AN-ACC Assessment Age. This figure represents the number of AN-ACC classification claims that have not been reviewed or reclassified within the last 12 months.
- As of September 2023, the AN-ACC Age has increased to 59.28%.
- This indicates that almost two–thirds of aged care residents have not had their service type or care needs reevaluated in over a year.
- Funding and rostering requirements could therefore be outdated if resident care needs have improved – or worsened.
- Basic reporting with claims data from Medicare could better influence the funding and rostering requirements to provide more up-to-date information.
“These data insights can help build accurate scenarios to align with care minute mandates, particularly when reclassification can take weeks if not months. It would allow you to avoid over-extension and not be in breach of your care time requirements,” Mr Covino added.
With a 10% band of influence and variance for funding and care minutes, there would be beneficial gains if timely AN-ACC reclassification occurred, and it could be the key to a three, four or five-star rating.
You can watch the full monthly highlight presented by Robert Covino on Mirus Australia’s website.