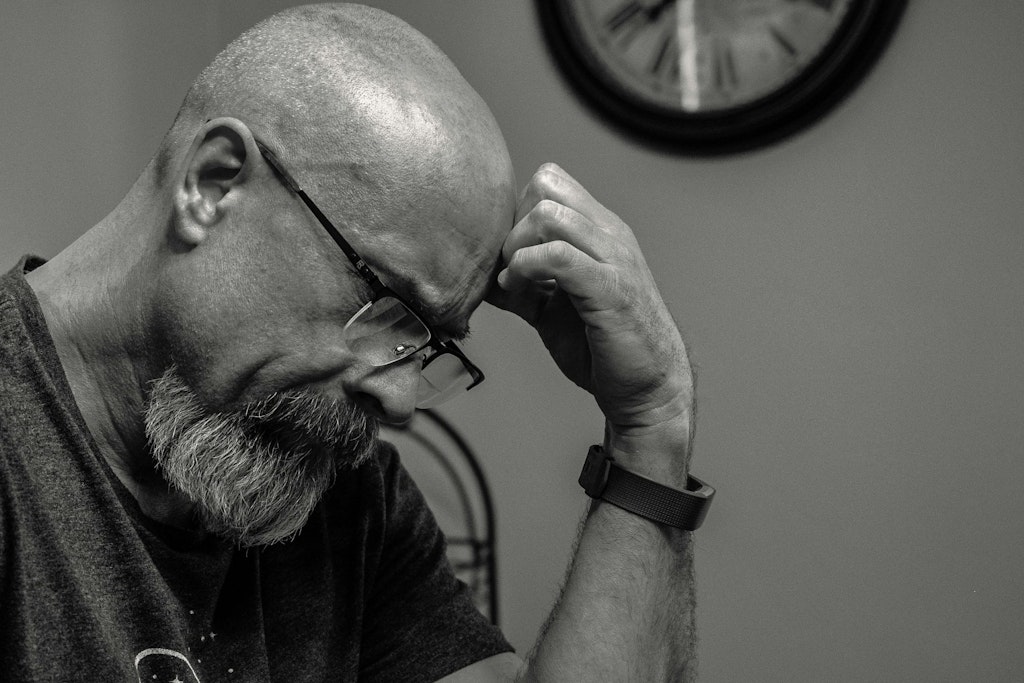
No finish line, no support, no hope- caregiver burnout needs attention, awareness and change
Last updated on 28 July 2025
It’s estimated that millions of people across the globe are silently caring for a loved one at any given time. From being the ‘nurse’, to ‘an assistant’, to ‘driver’ or ‘advocate’, daughters, sons, spouses and even friends are shouldering the burden of regular, and oftentimes, being singular point-person carer for people in their lives.
Having flown under the radar for decades, with many understanding care to be unquestionable “just doing the right thing”, “it’s expected of me” and “there’s no one else”. Slowly coming to the surface through social media, and now scientific research studies, is an epidemic of stressed and sick caregivers who aren’t coping with the prolonged and focussed responsibility of care.
Care-Giver Syndrome Deserves Awareness
Mel Robbins, a popular social media personality and advocate, has been fielding countless emails from fans and subscribers across the wider U.S and abroad. She is consistently hearing stories of hopelessness, stress and loneliness from people in their caregiving roles.
Carer burnout, or “caregiver syndrome” as its been coined, is not only coming to the fore from social media, the growing issue has come to the attention of medical academics globally. Organised studies have been conducted to gain insight into this growing trend. Multidisciplinary teams are trying to understand the formerly overlooked impacts on mental as well as physical health on the carer, and importantly, to provide options to alleviate the oftentimes severe symptoms that are exhibiting from burnout.
It’s important to understand that care-giver strain is not limited to professionals. In the multiple studies conducted, both professional and home settings were monitored. The strain of care over time impacted both those with and without formal degrees. Caring can also come in many forms, from parent to child, and child to parent, from sibling to sibling, and more or multiple threads of each.
Spotting Care-Giver Syndrome
Particularly dangerous is that many carers don’t see themselves as carers, exacerbating the hidden nature of the Syndrome, yet many are using up mental, physical and financial resources to care. Through societal norms and expectations, caring for children and caring for elderly parents, can be perceived as mandatory and expected. Through seeking to meet these societal and cultural expectations, many have brushed acknowledging that they are outlying huge personal resources to meet others’ needs and missing that they themselves are being impacted.
Robbins’ discussed the Syndrome with three physicians on her podcast. Through the discussion she unpacked the subtleties that lead to burnout and how easy it was for carers to get to that point due to the insidious nature of build-up. Their conversation highlights that a good start is to discern whether a person’s health, mood and sense of self has started to warp and suffer.
Medical experts who have studied Care-giver Syndrome list out common symptoms to look out for.
· Difficulty processing and holding emotions: Emotional and physical fatigue.
· Distancing from formerly close relationships: family, friends and other loved-ones.
· Inability to enjoy previously anticipated activities.
· A pervasive feeling of helplessness and hopelessness.
· Fluctuations and changes in appetite and/or weight.
· Fluctuations in, and interrupted, sleep patterns.
· Difficulty concentrating
· Increased illness and sickliness
· A difficulty moderating temper: increased frustration or irritability and/or anger toward others.
Minimising can be damaging
Robbins and her expert guests emphasise that it can be bizarre, perpetually feeling tired after a full nights’ sleep; Suddenly keeping on top of your household, and basic life admin, starting to feel like a gargantuan task that is simply too complicated.
In studies, a pervasive theme is exhaustion and irritability, not only with others but yourself, wanting to do more and being frustrated that everything can’t be achieved in the day. This constant pushing, from an energy ‘tank’ that is empty leads to only further burn-out and impacts on mental and physical health.
From her conversation with the medical team, Robbins puts it that “you’re irritable and short-tempered because you’re fried from taking care of everybody else.” In her discussion with these physicians, it is the insidious nature of minimising symptoms that can lead to further burnout. Where increased illness and sickliness is explained away, “oh the allergy season is particularly bad this year” and “the lack of interest in activities you used to love can really creep up on you.”
They also highlight that many carers are “so worn down [they perceive] their needs don’t matter” and troublingly many “feel guilty when [they] want to take time for [themselves]”.
Intensified stress
1. Stress can feel acute when it is felt alone. It is the feeling that you are the only one in this, that it is all up to you, and while you can be surrounded by people in your day you feel alone in this shouldering this care responsibility.
2. Chronic: Studies show that the strain and stress from caregiving doesn’t end for months, years or even decades – it’s chronic, and many who are in it see no finish line.
3. Care reshapes relationships – Through the shift to caring, a person is no longer just daughter, parent or spouse, they become “the nurse, the advocate, the driver.” There is perceived expectation to keep it all together which results in changed and strained relationships. This is another change that the carer has to manage, grief and adapt to.
Countless studies and Robbins speak to the significant changes that must be made for carers across the world, from psychological tools to equip carers to manage their mental health to systemic changes, much is called for. Robbins speaks to this, the consistent trend of guilt, and failure being written to her by fans, she says “what really bothers me is that you’re making yourself wrong over it, that ends today.”
Reaching out daily is hugely beneficial
Research has conclusively found that speaking about difficulties or struggles we are having through small daily interactions with friends and/or family can have a definitive improvement in our mental well-being, which can flow through to physical improvement.
A combined study across three U.S universities found that having a small conversation with a friend each day had the power to impact a person’s ability to find mental stamina and perseverance. Having the opportunity to be heard, be understood and empathised with was shown to have a significant impact on loneliness.
Even if it’s a 10 minute conversation with a friend in the car, reaching out vocally with where you’re at in your caring journey can be a vital step to eradicating loneliness in the caring journey.
Asking for help
Medical experts advise that if even if you have just an inkling that you may be experiencing carer burnout, don’t dismiss it but feel emboldened to reach out and overtly ask for help. Your current support network may not realise you are struggling.
Importantly however, as well as informal requests for help to friends, to seek consistent professional help, whether a psychologist or counsellor is highly encouraged by the academic and medical communities. Navigating burnout with support has been a critical component of improvement and strength for many.
Not only does it provide the opportunity to have your concerns validated by an external source, it can provide techniques and tools to improve thinking, approaching and managing the caring responsibility.
Respite Care is vital
Physicians and researchers greatly recommend that people seek formal systems and resources of help. Federally and across all states in Australia, there are respite services offered to help shoulder the responsibility of care.
Respite care is the temporary but consistent break for primary caregivers, to allow for a removal from the care position, to focus on themselves and self-care for a time.
Critically when it comes to managing carer burnout, the first step is the acknowledgement that it may be happening. To give space to go through the symptoms and assess if they are detrimentally affecting the way that life is lived.
The next step is to be encouraged and know the justification in reaching out and clearly articulating that you are struggling. Whether it’s to family members and friends, feeling alone and unheard is damaging mentally and physically.
And lastly, to seek formal resources for respite care, in providing moments to step away from the care-giving role; to decompress, manage self-care and be grounded in your sense of self are opportunities that all deserve.